Mental Health & Substance Abuse Billing Service
Content

Part of mastering billing and understanding insurance coverage is distinguishing between in-network and out-of-network. Work flexible hours as part of a supportive virtual community of care providers. Luckily, there are many options available for you to bill insurance. You can outsource the entire thing, use practice management software designed specifically for therapists, or do it yourself. Thank you for substantially helping with this difficult aspect of my practice. I appreciate all your help and the patients are grateful for your courtesy…
- We recommend using one EHR software, ideally custom built only for mental health providers, to manage all your clients in one place, and to submit all your appointments through one website.
- And this, of course, can be a patient dissatisfier at times when they receive insurance denials.
- We do this for free, but here is a guide and script on how to do eligibility and benefits calls yourself.
- The companies and their insurers warned that the rules could create “unnecessary burdens” for providers, insurers and patients, and “unintentionally” impede access to care.
- Every provider we work with is assigned an admin as a point of contact.
There’s plenty to know about this cycle, but for now, here’s an overview of the basic steps. When considering whether to join a network or accept payment from insurers, it’s important to evaluate their pre-approval rules and their mental health billing limits for payment. In some cases, the low payments and hassles of dealing with insurers make it more profitable to switch to a cash-only model and accept lower payments from clients or establish an income-based sliding scale.
Page Help for Article – Billing and Coding: Psychiatry and Psychology Services (A
You now have all the necessary information to file claims, you know what to charge the patient in person, and you know where to file the claims. If you need more information on coverage, contact the Medicare Administrative Contractor (MAC) who published the document. The contractor information can be found at the top of the document in the Contractor Information section (expand the section to see the details). If you are looking for a specific code, use your browser’s Find function (Ctrl-F) to quickly locate the code in the article. Sometimes, a large group can make scrolling thru a document unwieldy. You can collapse such groups by clicking on the group header to make navigation easier.
In the mental health field, patients and insurers are billed primarily for therapy, medical management and psychological testing services. Insurers have rules about how long a session they’ll pay for, how many they’ll pay for per day or week, and often a maximum number of treatments that they will pay for. The mental health needs of the patient may exceed the services the insurer is willing to pay for, making balancing an effective treatment plan with adequate reimbursement tough for mental health professionals. Psychiatrists, psychologists and therapists can improve their collection rate by hiring trained staff who understand billing for mental health services and the ins and outs of the insurance industry. The extra cost of hiring someone will be offset by the increase in revenue from seeing more patients and building your practice.
Assessment of Aphasia and Cognitive Performance Testing CPT Codes
Everything transpiring between a patient and the mental healthcare provider should be in the medical record. A patient’s medical record determines what is billed for the mental health service, which means that all required information must be adequately documented. This medical record will help support the diagnosis and procedure code that is billed to insurance.
But we still face issues with payers understanding and recognizing that this is medical and not behavioral health. And this, of course, can be a patient dissatisfier at times when they receive insurance denials. But this particular assessment is very interesting because again, it’s a blend of the medical and the psychological issues. So with these codes, they’re designed to identify and address psychological, behavioral, emotional, cognitive, interpersonal factors important to the assessment, treatment or management of physical health problems.
Billing and Coding: Psychiatry and Psychology Services
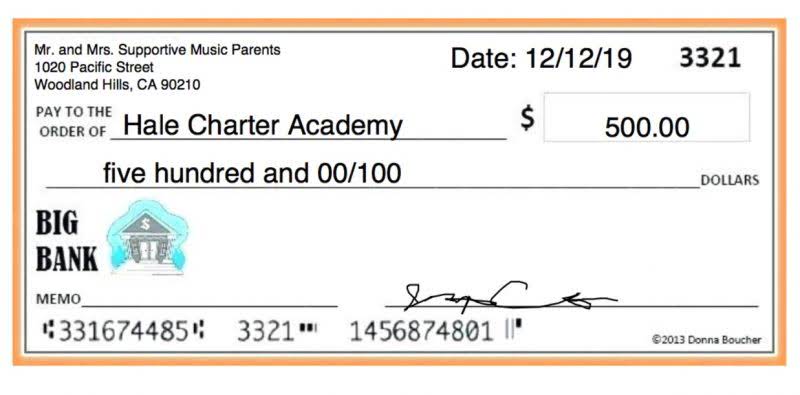
You are to charge them after the fact for their patient responsibility payment per session as listed on the completed EOB your receive from filing your claims. Call up the phone number on the back of their insurance card and begin the process of verifying eligibility and benefits. A claim that uses previous billing information to make changes to future billing for that same service date. The process by which you fill out a CMS1500 form with your client’s demographic and insurance information, your provider information, and the appointment information.
- If you went this route it would take you a few years to get a grasp on all of the jargon.
- So they’re designed to add on to another service that you may be performing.
- The best way to handle payments with clients is by being transparent.
- Information on Medicaid reimbursement for telehealth by state is available at the Center for Connected Health Policy with live policy trend maps.
- One is for physicians and qualified health care professionals, and the second set is for groups that we term of qualified non-physicians.
Also perform a new eligibility and benefits check for that client from Chapter 2 of this mental health billing for dummies guide. Make sure you’re filing claims to the right place, with the right information. You don’t have to when using a reputable mental health insurance billing service. We get it, it’s why we created a mental health insurance billing service after all.
Now, in this case, the patient’s primary diagnosis is physical in nature, but the assessments are meant to address the psychological impacts on those particular disease states and amelioration. The different codes are for either an individual, you’re working with a group, you’re working with a family, or family settings. So there are a number of options that are available, but I didn’t particularly want to call that one out, because again, it’s a blend of medical and the psychological areas, and the codes are specifically designed to do that. The last one I’ll call out is really on the far side, when we really good over to Collaborative Care.


